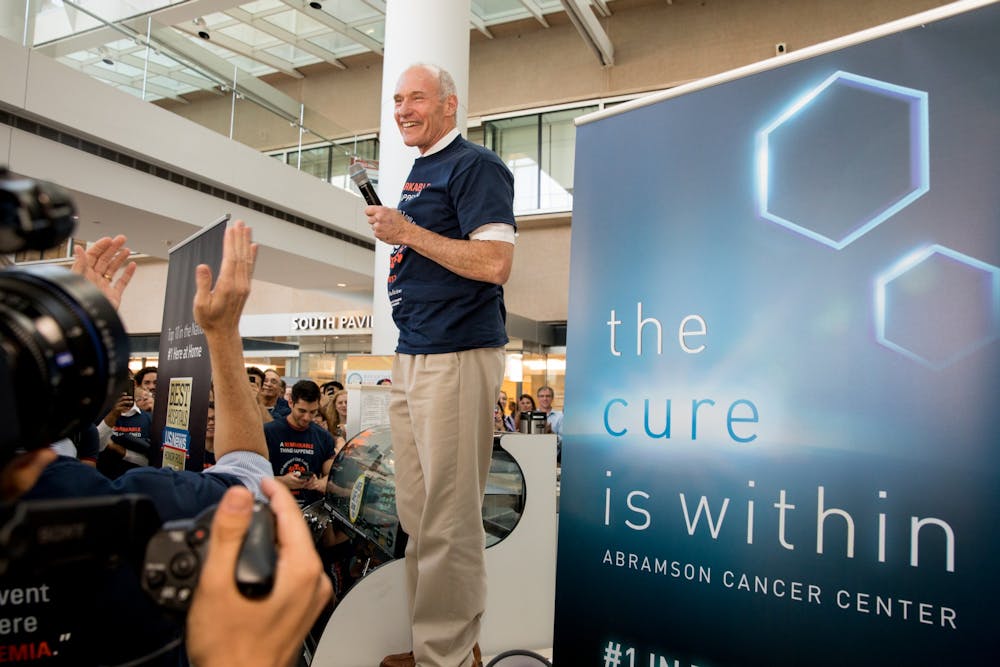
Perelman School of Medicine professor Carl June won the 2021 Dan David Prize for his work on the first United States Food and Drug Administration-approved personalized cellular therapy for cancer treatment.
June, the director of the Center for Cellular Immunotherapies at Penn, will share the $1 million prize with two other scientists, Zelig Eshhar and Steven Rosenberg, who he worked with to revolutionize the use of chimeric antigen receptor T-cell therapy to treat patients with cancer. CAR T-cell therapy is a treatment in which a patient's T-cells, a type of white blood cell important to a human's immune response, are modified to attack cancer cells.
The Dan David Prize annually rewards achievements that have an outstanding scientific, technological, cultural, or social impact on the world. National Institute of Health Director Anthony Fauci, who has played a significant role in the United States' COVID-19 response, was another one of this year's winners.
"Cell therapy was one of the best examples of a technology that was promised but no one ever thought it could be commercialized," June said. "It was going to just be a boutique demonstration that could change the immune system, but no one thought it would be FDA approved."
After 15 years of research, the FDA recognized June's work as a "Breakthrough Therapy" for successful treatment of a life-threatening disease, and the newly branded drug Kymriah became the first personalized cellular therapy for cancer.
William Ludwig, the very first recipient of June's treatment and a survivor of leukemia, died on Jan. 31 at age 75 from pneumonia related to COVID-19. June praised Ludwig for his "altruistic generosity" to the scientific community in an email to The Philadelphia Inquirer on Wednesday.
June's T-cell treatment is also now available to children. In April 2012, seven-year-old cancer patient Emily Whitehead became the first child to receive June's experimental treatment at The Children's Hospital of Philadelphia after her cancer relapsed for the second time.
June said he was inspired to research CAR T-cell therapy after his first patient ever experienced liver failure after a bone marrow transplant.
RELATED:
Penn Med study finds that cancer patients in remission risk serious illness from COVID-19
Penn Medicine implements program to address structural racism in healthcare
“It was amazing to see how an incoming small amount of T-cells could have a mass effect over the liver, which weighs over a couple of pounds,” June said. “This was a powerful demonstration of how T-cells could completely wipe out an organ.”
Recently, June has joined worldwide efforts to find therapies to combat long-term lung damage caused by COVID-19 after recovering from the virus himself. Actemra, the drug his team used to counteract immune system overstimulation caused by T-cell therapy, has been in clinical trials for COVID-19 treatment.
He is currently sponsoring a project led by Emily Blumberg, the program director of the Infectious Disease Fellowship and professor of Medicine at the Hospital of the University of Pennsylvania, to use cyclosporine, an immunosuppressive drug used to prevent organ rejection after a transplant, in clinical trials to prevent the immune system from shutting down when exposed to COVID-19.
June said he hopes that young scientists understand that the end results of research are rewarding, even if the process comes with unexpected disappointments and bumps in the road along the way.
"Your career will change and there will be many forks down the road," June said. "You have to consider the unexpected opportunities even if they are disappointing and take them. Recognize the good out of the accidents."